Health care costs are about to skyrocket for Americans in marginalized communities
It appears unlikely that Congress will prevent the expiration of enhanced premium tax credits (EPTCs) before a new year of coverage in the Affordable Care Act (ACA) marketplace begins on January 1, 2026. The average increase in health insurance costs is projected to exceed $1,000 a year for more than 20 million people who use these tax credits to help pay insurance premiums.
The expiration of EPTCs is not the only blow suffered by people who buy ACA insurance. Changes enacted by the budget law passed by the Republican majorities in the House and Senate and signed into law by President Trump, as well as policies adopted by the Trump administration, have increased paperwork burdens that make enrollment and renewal more difficult, eliminated coverage for lawfully present immigrants and dramatically reduced the level of assistance people receive to help them obtain and retain ACA insurance.
Americans from all backgrounds will be negatively affected, unless Congress extends EPTCs and retracts other recent cuts to ACA coverage. But Latinos and other people from historically marginalized communities will suffer disproportionate harm. They are particularly likely to need and qualify for ACA insurance, as many work in jobs that do not offer health benefits and earn too much to qualify for Medicaid but too little to afford health insurance on their own.
Here, we analyze the distribution of ACA enrollment by race and ethnicity and find that an estimated 52% of marketplace enrollees are people of color, including:
- 6.5 million Latinos (27% of all ACA marketplace enrollees).
- 3.6 million African Americans (15%).
- Nearly 2 million AANHPI people (8%).
- More than 100,000 Native Americans (1%).1
Analysis
Unfortunately, one cannot simply rely on administrative data showing self-reported race and ethnicity. Based on KFF tabulations of self-reported race and ethnicity, 50% of marketplace enrollees decline to state those characteristics. Fortunately, this limitation can be overcome based on other data sources. As explained below, the precise approach varies between insurance offered through the federal healthcare.gov platform and state-based marketplace (SBM) insurance, which is offered on platforms operated by each state.
Keep up with the latest from UnidosUS
Sign up for the weekly UnidosUS Action Network newsletter delivered every Thursday.
Healthcare.gov coverage
In publications released through October 2024, the Department of Health and Human Services (HHS) Assistant Secretary for Planning and Evaluation (ASPE) overcame the limitations of self-reported demographics in healthcare.gov data. For those who declined to provide information about race and ethnicity, ASPE imputed those characteristics, based on other available information about each enrollee. ASPE concluded that in 2024 (the last year for which these imputations are available), almost 55% of enrollees in healthcare.gov plans were people of color (Figure 1).
Figure 1. Healthcare.gov enrollees, by race and ethnicity: 2024
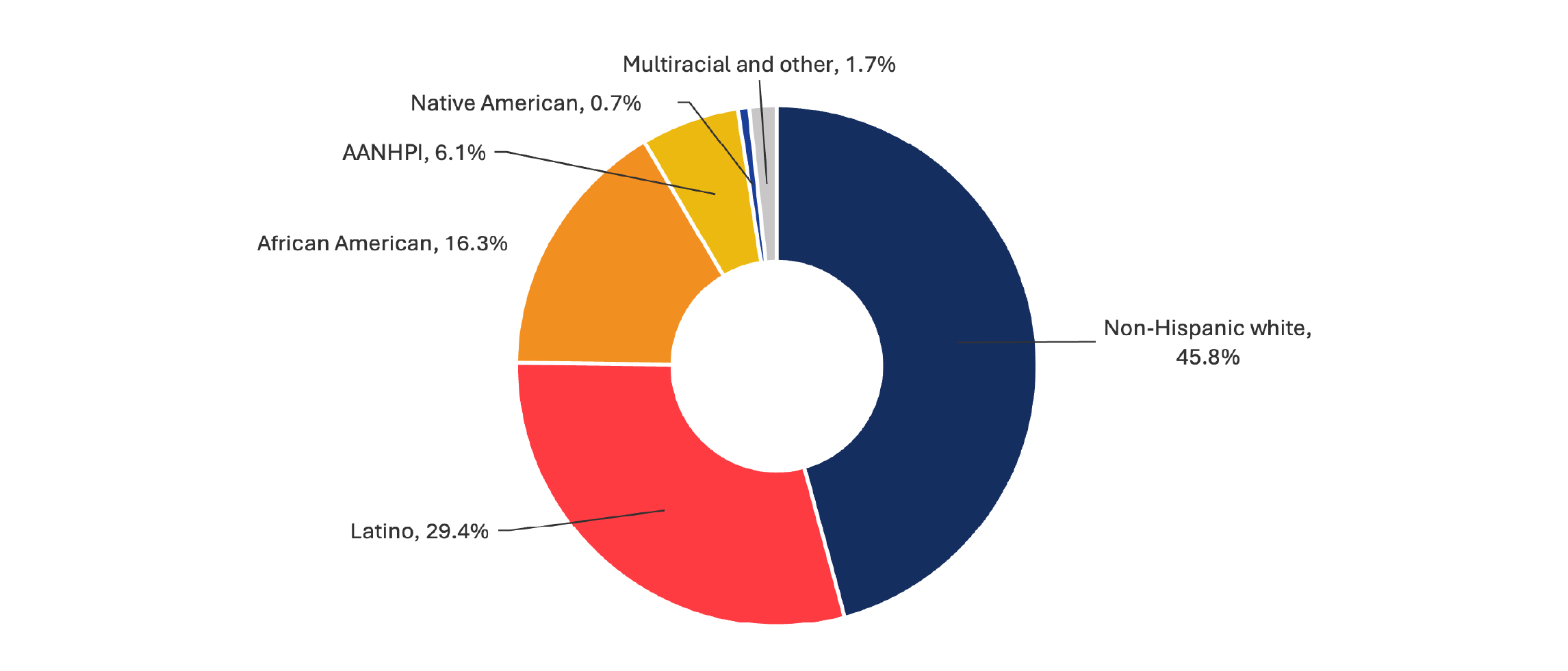
Source: ASPE, October 1, 2024.
Note: Latinos are Hispanics of all races. All other designations are limited to non-Hispanics. AANHPI = Asian Americans, Native Hawaiians and Pacific Islanders. Totals may not sum because of rounding.
SBM coverage
Unfortunately, no similar study imputes race and ethnicity into the administrative totals of marketplace enrollees in SBM states. Earlier this year, the Trump administration released open enrollment public use files showing that, in 2025, 17.1 million people enrolled in healthcare.gov plans and 7.2 million people enrolled in ACA plans offered by SBMs in 19 states and the District of Columbia.2
Current Population Survey-Annual Social and Economic Supplement (CPS-ASEC) data provides reliable information about survey respondents’ race and ethnicity. To estimate race and ethnicity among ACA enrollees in SBM states, we rely on CPS-ASEC data showing the racial and ethnic characteristics of people who describe themselves as enrolled in marketplace coverage in 2025 SBM states. Using this measure, we estimate that people of color comprise nearly half (47%) of SBM enrollees (Figure 2).
Figure 2. People who buy their own ACA coverage in SBM states, by race and ethnicity, 2025
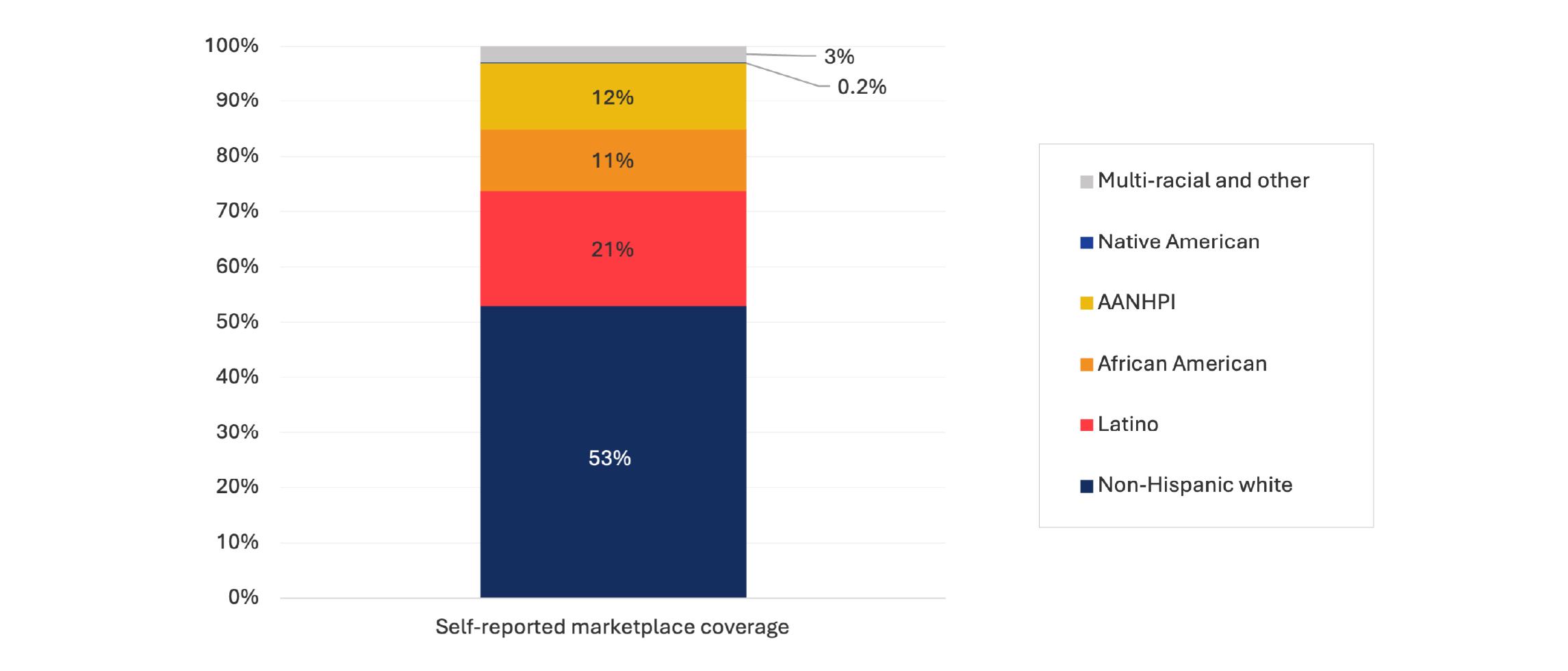
Source: UnidosUS analysis of 2025 CPS-ASEC data, accessed via IPUMS USA, University of Minnesota, www.ipums.org.
Note: Latinos are Hispanics of all races. All other designations are limited to non-Hispanics. AANHPI = Asian Americans, Native Hawaiians, and Pacific Islanders. Totals may not sum because of rounding. The states included as SBM states are all the SBM states indicated in HHS’s Public Use Files for Open Enrollment 2025.
Combining healthcare.gov and SBM estimates
To estimate the total number of marketplace enrollees in healthcare.gov states, by race and ethnicity, we apply the proportionate distribution found by ASPE to the total number of 2025 enrollees in healthcare.gov states. We similarly apply the proportionate distribution estimated based on CPS-ASEC data to the total number of 2025 enrollees in SBM states. We conclude that an estimated 52% of all marketplace beneficiaries in 2025 are people of color, including 6.5 million Latinos, 3.6 million African Americans, 1.9 million AANHPI people and more than 100,000 Native Americans (Table 1).
Table 1. Estimated distribution of ACA marketplace enrollees by race, ethnicity, and source of marketplace coverage: 2025 (millions)
| Non-Hispanic white | Latino | African American | AANHPI | Native American | Multiracial and other | Total | |
| Healthcare.gov states | 7.8 | 5.0 | 2.8 | 1.0 | 0.12 | 0.3 | 17.1 |
| SBM states | 3.8 | 1.5 | 0.8 | 0.9 | 0.012 | 0.2 | 7.2 |
| Total number | 11.7 | 6.5 | 3.6 | 1.9 | 0.13 | 0.5 | 24.3 |
| Total percentage | 48% | 27% | 15% | 8% | 1% | 2% | 100% |
Sources: UnidosUS analysis of HHS Public Use Files for Open Enrollment 2025. See also sources and notes for Figures 1 and 2, above.
Note: Latinos are Hispanics of all races. All other designations are limited to non-Hispanics. AANHPI = Asian Americans, Native Hawaiians and Pacific Islanders. Totals may not sum because of rounding. The states included as SBM states are those described as such in the 2025 Public Use Files.
Conclusion
Millions of Americans are struggling with unaffordable costs for everyday necessities, including food, housing, energy bills and health care. The last thing they need is a sudden spike in health insurance costs — but that is exactly what they are about to endure, unless Congress finally decides to extend the health insurance tax credits that are scheduled to expire after 2025.
People of all races and ethnicities will pay a heavy price, but an especially steep price will be paid by America’s Latinos, along with others from historically marginalized communities.
1 These percentages do not sum to 100% because of rounding and because they do not include people who are of other races or multiracial.
2 For 2025, 20 state-level jurisdictions operate SBMs: California, Colorado, Connecticut, the District of Columbia, Georgia, Idaho, Kentucky, Maine, Maryland, Massachusetts, Minnesota, Nevada, New Jersey, New Mexico, New York, Pennsylvania, Rhode Island, Vermont, Virginia, and Washington.



